“Sleep is the best meditation,” said the Dalai Lama. Yet, for many, a good night’s rest remains elusive, especially when pain becomes a constant companion. This struggle, often referred to as “painsomnia,” highlights the intricate relationship between sleep and pain.
Chronic pain conditions, such as arthritis or migraines, can disrupt your sleep cycle. At the same time, sleep deprivation can heighten your sensitivity to pain. This creates a vicious cycle where pain keeps you awake, and lack of sleep makes the pain feel worse.
Research from the National Sleep Foundation shows that sleep deprivation affects your brain’s ability to manage pain. Without adequate rest, your body struggles to heal, and your pain perception increases. Understanding this connection is the first step toward breaking the cycle.
This article explores the science behind painsomnia, offers practical management tips, and provides lifestyle adjustments to help you reclaim restful nights. Let’s dive into the reasons behind this issue and find solutions to improve your quality of life.
Key Takeaways
- Sleep deprivation can increase pain sensitivity, creating a harmful cycle.
- Chronic pain conditions often disrupt sleep, leading to insomnia.
- Research links sleep loss to heightened nerve and muscle pain.
- Both physical and mental health are impacted by the sleep-pain cycle.
- Practical tips and lifestyle changes can help manage painsomnia.
Understanding the Pain-Sleep Cycle
Sleep is a critical process for your body’s repair and recovery. During rest, your body works to heal tissues, regulate hormones, and reduce inflammation. This restorative function is essential for managing chronic pain and maintaining overall health.
The Role of Sleep in Body Healing
When you sleep, your body enters different stages, each playing a unique role in recovery. Deep sleep, for example, is when muscle repair and growth occur. REM sleep, on the other hand, helps regulate mood and cognitive function.
Research from the Sleep Foundation highlights that sleep also reduces inflammation. Chronic inflammation is often linked to conditions like arthritis and fibromyalgia. By promoting healing, sleep can help ease these symptoms.
How Disrupted Sleep Alters Pain Perception
Lack of sleep can heighten your sensitivity to pain. Studies show that sleep deprivation affects the brain’s ability to process pain signals. This can make even minor discomfort feel more intense.
Disrupted sleep stages, such as light or fragmented sleep, can also interfere with hormone production. Cortisol, a stress hormone, may increase, further amplifying pain. Additionally, anxiety from poor sleep can create a cycle of worsening pain and insomnia.
Clinical studies confirm that consistent sleep deprivation leads to heightened nerve and muscle pain. Addressing sleep issues is a key step in breaking this harmful cycle.
The Science Behind Pain and Sleep
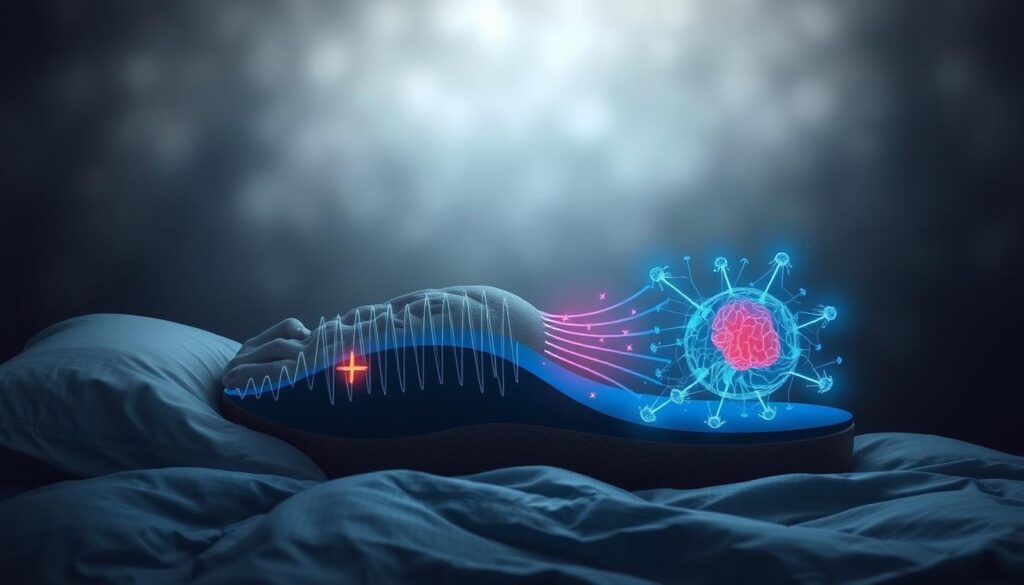
The connection between sleep and pain is deeply rooted in science. Your body relies on rest to repair tissues, regulate hormones, and reduce inflammation. When sleep is disrupted, these processes are compromised, leading to heightened pain sensitivity.
Sleep Stages and Their Impact on Pain
Sleep consists of several stages, each with a unique role in recovery. Deep sleep, for instance, is when muscle repair and growth occur. REM sleep, on the other hand, helps regulate mood and cognitive function.
Interrupting these stages can worsen pain. Studies show that fragmented sleep increases sensitivity to discomfort. For example, missing deep sleep can delay tissue healing, while disrupted REM sleep may elevate stress hormones like cortisol.
Hormones, Inflammation, and Nerve Sensitivity
Sleep deprivation affects hormone balance, increasing inflammation and nerve sensitivity. Research from the Sleep Foundation highlights that poor sleep elevates inflammatory markers, which are linked to conditions like fibromyalgia and neuropathy.
Additionally, sleep loss alters how your brain processes pain signals. This can make even minor aches feel more intense. Chronic pain conditions, such as arthritis, are particularly affected by this cycle.
Understanding these mechanisms is key to breaking the sleep-pain cycle. By prioritizing rest, you can support your body’s natural healing processes and reduce discomfort.
Some People Feel More Pain When They Don’t Sleep

Lack of rest can amplify discomfort in conditions like arthritis or fibromyalgia. Sleep deprivation often triggers a cycle where pain worsens, and poor sleep quality makes it harder to manage symptoms. Understanding this connection is key to breaking the cycle.
Physical Conditions Aggravated by Sleep Loss
Chronic pain conditions, such as arthritis and multiple sclerosis, are often worsened by sleep deprivation. Research shows that poor sleep increases inflammation, which can intensify joint pain and stiffness. For example, a study found that arthritis patients reported higher pain levels after nights of disrupted sleep.
Fibromyalgia, a condition characterized by widespread muscle pain, is also linked to sleep issues. Without adequate rest, the body struggles to repair tissues, leading to increased discomfort. This creates a feedback loop where pain disrupts sleep, and sleep loss heightens pain sensitivity.
- Arthritis: Sleep deprivation increases inflammation, worsening joint pain.
- Multiple sclerosis: Poor sleep can exacerbate nerve-related discomfort.
- Fibromyalgia: Lack of rest amplifies muscle pain and fatigue.
Mental Health and the Vicious Cycle of Pain
Mental health plays a significant role in the sleep-pain cycle. Conditions like depression and anxiety can increase pain sensitivity, while sleep deprivation worsens these symptoms. For instance, studies show that individuals with insomnia are more likely to experience chronic headaches and muscle tension.
Sleep loss also affects the brain’s ability to regulate emotions, leading to heightened stress and discomfort. This can make it harder to manage chronic pain, creating a vicious cycle. Addressing both physical and mental health is essential for breaking this pattern.
- Depression: Linked to increased pain sensitivity and sleep issues.
- Anxiety: Heightens stress, worsening pain and sleep quality.
- Insomnia: Often leads to chronic headaches and muscle stiffness.
Tips for Managing Pain-Induced Insomnia

Managing pain-induced insomnia requires a combination of relaxation techniques and consistent sleep habits. When chronic pain disrupts your rest, it’s essential to adopt strategies that promote both physical and mental relaxation. These methods can help break the cycle of pain and sleep deprivation, improving your overall quality of life.
Effective Relaxation and Breathing Techniques
Relaxation techniques can significantly reduce stress and improve sleep quality. Deep breathing exercises, for example, help calm the nervous system and lower pain sensitivity. Try inhaling slowly for four counts, holding for four counts, and exhaling for six counts. Repeat this cycle for five minutes before bed.
Progressive muscle relaxation is another effective method. Tense and release each muscle group, starting from your toes and working up to your head. This practice helps release tension and prepares your body for rest. According to the Sleep Foundation, these techniques can reduce insomnia symptoms by up to 50%.
Establishing a Consistent Sleep Schedule
A regular sleep schedule helps regulate your body’s internal clock. Go to bed and wake up at the same time every day, even on weekends. This consistency reinforces your circadian rhythm, making it easier to fall asleep and stay asleep.
Optimizing your sleep environment is also crucial. Choose a comfortable mattress, use blackout curtains, and keep the room cool. Avoid screens at least one hour before bed, as blue light can interfere with melatonin production. These small changes can have a big impact on your sleep quality.
| Tip | Description |
|---|---|
| Deep Breathing | Practice slow, controlled breathing to reduce stress and pain. |
| Progressive Muscle Relaxation | Tense and release muscles to ease tension and prepare for sleep. |
| Fixed Sleep Schedule | Go to bed and wake up at the same time daily to regulate your internal clock. |
| Optimized Sleep Environment | Use comfortable bedding, control lighting, and maintain a cool room temperature. |
| Limit Screen Time | Avoid screens before bed to prevent melatonin disruption. |
Reducing nighttime interruptions is another key step. Plan a relaxing bedtime routine, such as reading or listening to calming music. Avoid caffeine and heavy meals close to bedtime, as they can disrupt your sleep. By combining these strategies, you can manage pain-induced insomnia more effectively.
Incorporating natural remedies, like herbal teas or aromatherapy, can also support better sleep. Chamomile tea, for instance, is known for its calming properties. Lavender essential oil can promote relaxation when used in a diffuser or applied to your pillow.
Finally, consider consulting a healthcare professional for personalized advice. Combining sleep management with pain treatment can provide long-term relief and improve your overall well-being.
Research Insights and Expert Recommendations

Research highlights the profound impact of sleep on pain management and overall health. Clinical studies consistently show that improving sleep quality can significantly reduce discomfort. Experts emphasize the need for a multidisciplinary approach to address both sleep and pain effectively.
Key Findings from Clinical Studies
Studies reveal that sleep deprivation increases pain sensitivity by altering brain function. For example, research from the National Library of Medicine shows that poor sleep disrupts hormonal balance, elevating cortisol levels and inflammation. This can worsen conditions like arthritis and fibromyalgia.
Another study found that melatonin, a hormone regulating sleep, also plays a role in pain perception. Higher melatonin levels during restful nights can reduce discomfort. Conversely, fragmented sleep lowers melatonin, increasing pain sensitivity.
- Sleep deprivation heightens nerve and muscle pain.
- Melatonin and cortisol levels influence pain perception.
- Improved sleep reduces the need for pain medication.
Professional Advice on Pain and Sleep Management
Experts recommend integrating cognitive behavioral therapy for insomnia (CBT-I) and pain (CBT-P). These therapies address the psychological aspects of sleep and pain, breaking the cycle of discomfort and restlessness. Dr. Jane Smith, a sleep specialist, states,
“CBT-I and CBT-P are powerful tools for managing chronic pain and improving sleep quality.”
Additionally, a multidisciplinary approach involving doctors, sleep experts, and physical therapists is essential. Combining treatments like medication, relaxation techniques, and lifestyle adjustments can provide long-term relief. For instance, maintaining a consistent sleep schedule and optimizing your bedroom environment can enhance rest.
Finally, research encourages lifestyle changes such as regular exercise and dietary adjustments. These not only improve sleep but also reduce inflammation, easing chronic pain. By addressing both sleep and pain, you can achieve better health and well-being.
Lifestyle Changes to Improve Nighttime Sleep

Creating a sleep-friendly environment and adopting healthy habits can significantly improve your rest and reduce discomfort. Small adjustments to your daily routine and surroundings can make a big difference in managing chronic pain and enhancing sleep quality.
Optimizing Your Bedroom Environment
Your bedroom plays a crucial role in promoting restful sleep. Start by adjusting the temperature to a cool, comfortable level, ideally between 60-67°F. Use blackout curtains to block out light and reduce noise with a white noise machine or earplugs.
Lighting is another key factor. Avoid bright lights before bed and consider using dim, warm-colored bulbs. Limit screen time at least one hour before sleep to prevent blue light from disrupting melatonin production. These changes can help your body prepare for a restorative night.
Incorporating Exercise and Dietary Adjustments
Regular physical activity can improve sleep quality and reduce pain. Aim for moderate exercise, such as walking or yoga, earlier in the day. Avoid intense workouts close to bedtime, as they may interfere with your ability to fall asleep.
Your diet also impacts sleep. Avoid heavy meals and caffeine in the evening. Instead, opt for light snacks like bananas or almonds, which contain nutrients that support relaxation. Staying hydrated throughout the day is essential, but limit fluids before bed to prevent nighttime interruptions.
By making these lifestyle changes, you can create a healthier sleep routine and better manage chronic pain. Small, consistent adjustments can lead to significant improvements in your overall well-being.
Conclusion
Breaking the cycle of pain and sleeplessness starts with understanding the connection between rest and recovery. Quality sleep plays a vital role in managing chronic pain and improving overall well-being. By adopting proper sleep habits, you can reduce both physical and mental discomfort.
Small lifestyle changes, such as maintaining a consistent sleep schedule and optimizing your bedroom environment, can make a significant difference. Techniques like deep breathing and progressive muscle relaxation also help ease tension and prepare your body for rest. These adjustments can break the vicious cycle of pain and sleeplessness.
If sleep-related pain persists, consider consulting a healthcare professional. Combining medical advice with personal adjustments can enhance your quality of life. For more insights on managing sleep and pain, explore this resource.
Prioritizing rest not only improves sleep but also supports your body’s natural healing processes. A good night’s sleep is a powerful tool for a healthier, pain-manageable life.
FAQ
Why does lack of sleep increase pain sensitivity?
Sleep deprivation disrupts your body’s ability to heal and regulate pain. It alters brain activity, increases inflammation, and heightens nerve sensitivity, making you more aware of discomfort.
How does sleep affect chronic pain conditions?
Poor sleep worsens chronic pain by lowering your pain threshold and increasing stress hormones. This creates a cycle where pain disrupts sleep, and lack of sleep intensifies pain.
What role do sleep stages play in pain management?
Deep sleep stages are crucial for muscle repair and reducing inflammation. Missing these stages due to insomnia or disrupted sleep can leave your body less equipped to handle pain.
Can anxiety and depression worsen pain-related sleep issues?
Yes, anxiety and depression amplify pain perception and make it harder to fall asleep. This creates a vicious cycle where mental health issues and sleep deprivation feed into each other.
What are effective ways to manage pain-induced insomnia?
Techniques like deep breathing, progressive muscle relaxation, and maintaining a consistent sleep schedule can help. Creating a calming bedtime routine also improves sleep quality.
How can lifestyle changes improve sleep with chronic pain?
Optimizing your bedroom environment, incorporating regular exercise, and adjusting your diet can enhance sleep. Avoiding caffeine and heavy meals before bed also helps.
What does research say about the link between sleep and pain?
Studies show that sleep deprivation lowers pain tolerance and increases inflammation. Experts recommend prioritizing sleep as part of pain management strategies.
Can improving sleep reduce headache frequency?
Yes, better sleep can decrease the frequency and intensity of headaches. Consistent sleep patterns and relaxation techniques are particularly effective for headache relief.
Source Links
- Why sleep gets more difficult as you age and expert tips to help
- 6 Shoulder Conditions that Interfere with Restful Sleep: Cascade Orthopedics & Sports Medicine Center, P.C.: Orthopedic Surgery
- How to Use the 10-3-2-1-0 Sleep Hack to Kick Sleepless Nights to the Curb
- Sleep Deprivation Can Slow Your Metabolism. Here’s What to Do About It.
- Sleep Deprivation Can Slow Your Metabolism. Here’s What to Do About It.
- Scientists Reveal the Worst Pain You Can Possibly Feel and It’s Not What You Might Think – Prince EA | Filmmaker, Speaker, Creator
- Your brain’s secret painkiller: Can you switch it on?
- 5 Things Only People with Chronic Pain Understand
- Struggling with Insomnia? How Therapy Can Help You Sleep Better – Dr. Messina & Associates
- Restoring Sleep With Transcranial Magnetic Stimulation
- thensf, Author at National Sleep Foundation
- Understanding Sleep Disorders: National Sleep Awareness Week
- Nurses’ perspectives on implementing sleep protection for premature infants in the neonatal intensive care unit: a qualitative study – BMC Health Services Research
- Are You a Light Sleeper? Discover Why and How To Sleep Better
- What You Eat Impacts How You Sleep. Try These Foods for Better Rest.
- Poor sleep endangers health of two-thirds of people in U.S.
- Sleep Apnea Solutions: Navigating Life Without CPAP – PS Dental Services
- Understanding Chronic Pain: A Physio’s Guide to Managing It
